Throughout history, nothing has killed more human beings than infectious disease. Covid-19 shows how vulnerable we remain – and how we can avoid similar pandemics in the future.
The novel coronavirus pandemic, known as Covid-19, could not have been more predictable. From my own reporting, I knew this first-hand. In October 2019, I attended a simulation involving a fictional pandemic, caused by a novel coronavirus, that killed 65 million people, and in the spring of 2017 I wrote a feature story for TIME magazine on the subject. The magazine cover read: “Warning: the world is not ready for another pandemic”.
There was little special about my insight. Over the past 15 years, there has been no shortage of articles and white papers issuing dire warnings that a global pandemic involving a new respiratory disease was only a matter of time. On BBC Future in 2018, we reported that experts believed a flu pandemic was only a matter of time and that there could be millions of undiscovered viruses in the world, with one expert telling us, “I think the chances that the next pandemic will be caused by a novel virus are quite good.” In 2019, US President Donald Trump’s Department of Health and Human Services carried out a pandemic exercise named “Crimson Contagion”, which imagined a flu pandemic starting in China and spreading around the world. The simulation predicted that 586,000 people would die in the US alone. If the most pessimistic estimates about Covid-19 come true, the far better named “Crimson Contagion” will seem like a day in the park.
As of 26 March, there were more than 470,000 confirmed cases of Covid-19 around the world and more than 20,000 deaths, touching every continent save Antarctica. This was a pandemic, in reality, well before the World Health Organization finally declared it one on 11 March. And we should have seen it coming.
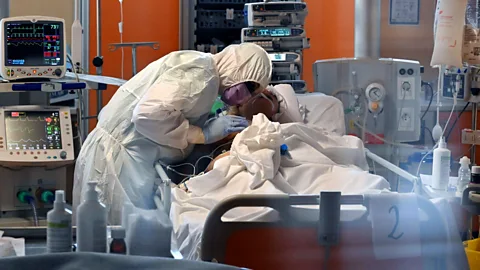 Getty Images
Getty ImagesCovid-19 marks the return of a very old – and familiar – enemy. Throughout history, nothing has killed more human beings than the viruses, bacteria and parasites that cause disease. Not natural disasters like earthquakes or volcanoes. Not war – not even close.
Mass killers
Take the mosquito-borne disease malaria. It has stalked humanity for thousands of years, and while death tolls have dropped significantly over the past 20 years, it still snuffs out nearly half a million people every year.
Over the millennia, epidemics, in particular, have been mass killers on a scale we can’t begin to imagine today – even in the time of the coronavirus.
You might also like:
The plague of Justinian struck in the 6th Century and killed as many as 50 million people, perhaps half the global population at the time. The Black Death of the 14th Century – likely caused by the same pathogen – may have killed up to 200 million people. Smallpox may have killed as many as 300 million people in the 20th Century alone, even though an effective vaccine – the world’s first – had been available since 1796.
Some 50 to 100 million people died in the 1918 influenza pandemic – numbers that surpass the death toll of World War One, which was being fought at the same time. The 1918 flu virus infected one in every three people on the planet. (Read more about how the 1918 flu changed the world). HIV, a pandemic that is still with us and still lacks a vaccine, has killed an estimated 32 million people and infected 75 million, with more added every day.
 Getty Images
Getty Images
Viral advantage
Pathogens make such effective mass killers because they are self-replicating. This sets them apart from other major threats to humanity. Each bullet that kills in a war must be fired and must find its target. Most natural disasters are constrained by area: an earthquake that strikes in China can’t directly hurt you in the UK.
But when a virus – like the novel coronavirus – infects a host, that host becomes a cellular factory to manufacture more viruses. Bacteria, meanwhile, are capable of replicating on their own in the right environment.
The symptoms created by an infectious pathogen – such as sneezing, coughing or bleeding – put it in a position to spread to the next host, and the next, a contagiousness captured in the replication number, or “R0” of a pathogen, or how many susceptible people one sick person can infect. (Imperial College London has estimated the novel coronavirus’s R0 at 1.5 to 3.5.) And because human beings move around – interacting with other human beings as they do so in every manner from a handshake to sexual intercourse – they move the microbes with them. (Read more about what makes viruses so difficult to outsmart).
No wonder militaries have long tried to harness disease as a tool of war. No wonder that, until recently, far more soldiers died of disease than died in combat. A pathogen is a perfectly economical weapon, turning its victims into its delivery system.
 Getty Images
Getty ImagesThe constant threat of disease, as much as any other factor, kept the reins on human development and expansion. At the dawn of the 19th Century, global life expectancy was just 29 years – not because human beings couldn’t live to much older ages even then, but because so many of us died in infancy from disease, or from infection during childbirth or after a wound. (Read more about whether our life spans are really longer than that of our ancestors).
The cities of the pre-modern era were only able to keep up their populations through a continual infusion of migrants to make up for citizens who died off from disease. The development first of sanitation, and then of countermeasures like vaccines and antibiotics, changed all that.
“The defeat of infection overcame these barriers and allowed us to have these great global cities,” says Charles Kenny, a senior fellow at the Center for Global Development, a think tank in Washington DC, and the author of the forthcoming book Winning the War on Death: Humanity, Infection and the Fight for the Modern World.
It was a victory that won us the modern world as we know it.
A better era
It can be difficult to comprehend how quickly that war was seemingly won. My great-grandparents could have fallen victim to the 1918 flu. My grandparents lived their infancy and youth before penicillin was developed. My parents were born before the polio vaccine was invented in 1954. Yet by 1962, the Nobel Prize-winning virologist Sir Frank Macfarlane Burnet could note that “to write about infectious disease is almost to write of something that has passed into history”.
In the developed world, and increasingly in the developing world, we are now far more likely to die from non-communicable diseases like cancer, heart disease or Alzheimer’s than from a contagion. The decline of infectious disease is the best evidence that life on this planet truly is getting better.
 Getty Images
Getty ImagesWhile reporting my book End Times, I visited the epidemiologist Marc Lipsitch at his office at the Harvard T.H. Chan School of Public Health in Boston one rainy morning in the spring of 2018. Lipsitch is one of the most influential epidemiologists in the United States, and one who takes seriously the possibility that disease pandemics might constitute a true global catastrophic risk – which is why I was there to see him.
But that morning Lipsitch showed me something I wasn’t expecting: a chart that graphed infectious disease mortality in the United States over the course of the 20th Century.
What it shows is a drastic decline, from around 800 deaths from infectious disease per 100,000 people in 1900 to about 60 deaths per 100,000 by the last years of the century. There was a brief spike in 1918 – that would be the flu – and a slight and temporary upturn during the worst of the AIDS epidemic in the 1980s. But, Lipsitch told me, “death rates from infectious disease dropped by nearly 1% a year, about 0.8 % per year, all the way through the century.”
Not over yet
That’s the good news. The bad news, as Covid-19 reminds us, is that infectious diseases haven’t vanished. In fact, there are more new ones now than ever: the number of new infectious diseases like Sars, HIV and Covid-19 has increased by nearly fourfold over the past century. Since 1980 alone, the number of outbreaks per year has more than tripled.
There are several reasons for this uptick. For one, over the past 50 years, we’ve more than doubled the number of people on the planet. This means more human beings to get infected and in turn to infect others, especially in densely populated cities. We also have more livestock now than we did over the last 10,000 years of domestication up to 1960 combined, and viruses can leap from those animals to us.
As Covid-19 is painfully demonstrating, our interconnected global economy both helps spread new infectious diseases – and, with its long supply chains, is uniquely vulnerable to the disruption that they can cause. The ability to get to nearly any spot in the world in 20 hours or fewer, and pack a virus along with our carry-on luggage, allows new diseases to emerge and to grow when they might have died out in the past.
For all the advances we’ve made against infectious disease, our very growth has made us more vulnerable, not less, to microbes that evolve 40 million times faster than humans do.
Antibiotics have saved hundreds of millions of lives since the serendipitous discovery of penicillin in 1928, but bacterial resistance to these drugs is growing by the year, a development doctors believe is one of the greatest threats to global public health. In fact, 33,000 people die each year from antibiotic resistant infections in Europe alone, according to a 2018 study. The “antibiotic apocalypse”, as England’s former chief medical officer, Sally Davies, called it, puts us in danger of returning to a time when even run-of-the-mill infections could kill.
Back in 2013, a World Bank estimate of how much the 1918 flu could cost our now much richer and more connected global economy put the figure at more than $4 trillion, nearly the entire GDP of Japan. Early estimates of the economic damage from Covid-19 have already crossed the trillion-dollar mark.
 Getty Images
Getty ImagesThe World Health Organization, which performed so well under the stress of Sars, has botched more recent outbreaks so badly that experts have called for the entire organisation to be overhauled. Climate change is expanding the range of disease-carrying animals and insects like the Aedes aegyptimosquitoes that transmit the Zika virus.
Even human psychology is at fault. The spread of vaccine scepticism has been accompanied by the resurrection of long-conquered diseases like measles, leading the WHO in 2019 to name the antivaccination movement one of the world’s top 10 public-health threats.
 Getty Images
Getty ImagesCovid-19 is very much a disease of the moment, emerging in a crowded city in a newly prosperous and connected China before spreading to the rest of the world in a matter of months. But our response to it has been both hyper-modern – and practically medieval. Scientists around the world are using cutting-edge tools to rapidly sequence the genome of the coronavirus, pass along information about its virulence, and collaborate on possible countermeasures and vaccines, all far quicker than could have been done before.
But when the virus arrived among us, our only effective response was to shut down society and turn off the assembly line of global capitalism. Minus the text alerts, the videoconferencing and the Netflix, what we were doing wasn’t that different from what our ancestors might have tried to halt an outbreak of the plague. The result has been chemotherapy for the global economy.
Just as the eventual emergence of something like Covid-19 was easily predictable, so too are the actions we should have taken to shore ourselves against its coming.
We need to strengthen the antennae of global health, to ensure that when the next virus emerges — which it will — we’ll catch it faster, perhaps even snuff it out. The budget of the WHO, the agency ostensibly charged with safeguarding the health of the world’s 7.8 billion citizens, is somehow no more than that of a large urban hospital in the U.S.
We need to double down on the development of vaccines, which will include assuring large pharma companies that their investments won’t be wasted should an outbreak end before one is ready.
 Getty Images
Getty ImagesWe need to build more slack into our public health systems. Just as the US military is designed — and funded — to fight a war on two fronts, so our health care systems should have the surge capacity to meet the next pandemic.
One ongoing challenge in pandemic preparation is what experts call shock and forgetting. Too often politicians make funding promises in the immediate aftermath of a crisis like Sars or Ebola, only to let those pledges lapse as the memory of the outbreak fades.
Somehow, I expect that won’t be the case with Covid-19. We need to do all we can to not just survive this pandemic, but to ensure it remains a throwback from the past, not a sign of things to come.
* Bryan Walsh is the Future Correspondent for Axios and the author of End Times: A Brief Guide to the End of the World, from which this story was adapted and updated. End Times is published by Hachette Books.
--
As an award-winning science site, BBC Future is committed to bringing you evidence-based analysis and myth-busting stories around the new coronavirus. You can read more of our Covid-19 coverage here.
--
If you liked this story, sign up for the weekly bbc.com features newsletter, called “The Essential List”. A handpicked selection of stories from BBC Future, Culture, Worklife, and Travel, delivered to your inbox every Friday.



Post a Comment